| Record Information |
|---|
| Version | 2.0 |
|---|
| Creation Date | 2009-06-09 20:08:59 UTC |
|---|
| Update Date | 2014-12-24 20:22:53 UTC |
|---|
| Accession Number | T3D0856 |
|---|
| Identification |
|---|
| Common Name | Oxalic acid |
|---|
| Class | Small Molecule |
|---|
| Description | Oxalic acid is a dicarboxylic acid. It is a colorless crystalline solid that dissolves in water to give colorless, acidic solutions. In terms of acid strength, it is much stronger than acetic acid. Oxalic acid, because of its di-acid structure can also act as a chelating agent for metal cations. About 25% of produced oxalic acid is used as a mordant in dyeing processes. It is also used in bleaches, especially for pulpwood. Oxalic acid's main applications include cleaning (it is also found in baking powder) or bleaching, especially for the removal of rust. Oxalic acid is found in a number of common foods with members of the spinach family being particularly high in oxalates. Beat leaves, parsley, chives and cassava are quite rich in oxalate. Rhubarb leaves contain about 0.5% oxalic acid and jack-in-the-pulpit (Arisaema triphyllum) contains calcium oxalate crystals. Bacteria naturally produce oxalates from the oxidation of carbohydrates. At least two pathways exist for the enzyme-mediated formation of oxalate in humans. In one pathway, oxaloacetate (part of the citric acid cycle) can be hydrolyzed to oxalate and acetic acid by the enzyme oxaloacetase. Oxalic acid can also be generated from the dehydrogenation of glycolic acid, which is produced by the metabolism of ethylene glycol. Oxalate is a competitive inhibitor of lactate dehydrogenase (LDH). LDH catalyses the conversion of pyruvate to lactic acid oxidizing the coenzyme NADH to NAD+ and H+ concurrently. As cancer cells preferentially use aerobic glycolysis, inhibition of LDH has been shown to inhibit tumor formation and growth. However, oxalic acid is not particularly safe and is considered a mild toxin. In particular, it is a well-known uremic toxin. In humans, ingested oxalic acid has an oral lowest-published-lethal-dose of 600 mg/kg. It has been reported that the lethal oral dose is 15 to 30 grams. The toxicity of oxalic acid is due to kidney failure caused by precipitation of solid calcium oxalate, the main component of kidney stones. Oxalic acid can also cause joint pain due to the formation of similar precipitates in the joints. |
|---|
| Compound Type | - Food Toxin
- Household Toxin
- Industrial/Workplace Toxin
- Metabolite
- Natural Compound
- Organic Compound
- Plant Toxin
- Reducing Agent
|
|---|
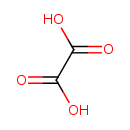
| Chemical Structure | |
|---|
| Synonyms | | Synonym | | Ammonium oxalate | | Ethane-1,2-dioate | | Ethane-1,2-dioic acid | | Ethanedioate | | Ethanedioic acid | | Ethanedioic acid dihydrate | | Ethanedionate | | Ethanedionic acid | | Kyselina stavelova | | Oxaalzuur | | Oxalate | | Oxalic acid 2-Hydrate | | Oxalic acid anhydrous | | Oxalic acid diammonium salt | | Oxalic acid dihydrate |
|
|---|
| Chemical Formula | C2H2O4 |
|---|
| Average Molecular Mass | 90.035 g/mol |
|---|
| Monoisotopic Mass | 89.995 g/mol |
|---|
| CAS Registry Number | 144-62-7 |
|---|
| IUPAC Name | oxalic acid |
|---|
| Traditional Name | oxalic acid |
|---|
| SMILES | OC(=O)C(O)=O |
|---|
| InChI Identifier | InChI=1S/C2H2O4/c3-1(4)2(5)6/h(H,3,4)(H,5,6) |
|---|
| InChI Key | InChIKey=MUBZPKHOEPUJKR-UHFFFAOYSA-N |
|---|
| Chemical Taxonomy |
|---|
| Description | belongs to the class of organic compounds known as dicarboxylic acids and derivatives. These are organic compounds containing exactly two carboxylic acid groups. |
|---|
| Kingdom | Organic compounds |
|---|
| Super Class | Organic acids and derivatives |
|---|
| Class | Carboxylic acids and derivatives |
|---|
| Sub Class | Dicarboxylic acids and derivatives |
|---|
| Direct Parent | Dicarboxylic acids and derivatives |
|---|
| Alternative Parents | |
|---|
| Substituents | - Dicarboxylic acid or derivatives
- Carboxylic acid
- Organic oxygen compound
- Organic oxide
- Hydrocarbon derivative
- Organooxygen compound
- Carbonyl group
- Aliphatic acyclic compound
|
|---|
| Molecular Framework | Aliphatic acyclic compounds |
|---|
| External Descriptors | |
|---|
| Biological Properties |
|---|
| Status | Detected and Not Quantified |
|---|
| Origin | Endogenous |
|---|
| Cellular Locations | - Cytoplasm
- Extracellular
- Mitochondria
- Peroxisome
|
|---|
| Biofluid Locations | Not Available |
|---|
| Tissue Locations | - Bladder
- Epidermis
- Eye Lens
- Fibroblasts
- Intestine
- Kidney
- Liver
- Pancreas
- Testes
|
|---|
| Pathways | | Name | SMPDB Link | KEGG Link |
|---|
| Primary Hyperoxaluria Type I | SMP00352 | Not Available | | Primary hyperoxaluria II, PH2 | SMP00558 | Not Available |
|
|---|
| Applications | Not Available |
|---|
| Biological Roles | |
|---|
| Chemical Roles | Not Available |
|---|
| Physical Properties |
|---|
| State | Solid |
|---|
| Appearance | White crystals |
|---|
| Experimental Properties | | Property | Value |
|---|
| Melting Point | 189.5°C | | Boiling Point | Not Available | | Solubility | 220 mg/mL at 25°C | | LogP | Not Available |
|
|---|
| Predicted Properties | |
|---|
| Spectra |
|---|
| Spectra | | Spectrum Type | Description | Splash Key | Deposition Date | View |
|---|
| GC-MS | GC-MS Spectrum - GC-EI-TOF (Pegasus III TOF-MS system, Leco; GC 6890, Agilent Technologies) (2 TMS) | splash10-0002-0900000000-eaa92cf80964dd7d345a | 2014-06-16 | View Spectrum | | GC-MS | GC-MS Spectrum - GC-EI-TOF (Pegasus III TOF-MS system, Leco; GC 6890, Agilent Technologies) (Non-derivatized) | splash10-0002-0900000000-b9206a3a54b5be6f07d9 | 2014-06-16 | View Spectrum | | GC-MS | GC-MS Spectrum - GC-EI-TOF (Pegasus III TOF-MS system, Leco; GC 6890, Agilent Technologies) (2 TMS) | splash10-00dj-9500000000-e5db327eab9e8a2f149e | 2014-06-16 | View Spectrum | | GC-MS | GC-MS Spectrum - GC-MS (2 TMS) | splash10-00sl-3910000000-75af6e42d4cc12d798f4 | 2014-06-16 | View Spectrum | | GC-MS | GC-MS Spectrum - EI-B (Non-derivatized) | splash10-0006-9000000000-8aef9a64d926571c2de0 | 2017-09-12 | View Spectrum | | GC-MS | GC-MS Spectrum - GC-EI-TOF (Non-derivatized) | splash10-0002-0900000000-eaa92cf80964dd7d345a | 2017-09-12 | View Spectrum | | GC-MS | GC-MS Spectrum - GC-EI-TOF (Non-derivatized) | splash10-0002-0900000000-b9206a3a54b5be6f07d9 | 2017-09-12 | View Spectrum | | GC-MS | GC-MS Spectrum - GC-EI-TOF (Non-derivatized) | splash10-00dj-9500000000-e5db327eab9e8a2f149e | 2017-09-12 | View Spectrum | | GC-MS | GC-MS Spectrum - GC-MS (Non-derivatized) | splash10-00sl-3910000000-75af6e42d4cc12d798f4 | 2017-09-12 | View Spectrum | | GC-MS | GC-MS Spectrum - GC-EI-TOF (Non-derivatized) | splash10-0002-0900000000-3cee49bf06349fbe625e | 2017-09-12 | View Spectrum | | Predicted GC-MS | Predicted GC-MS Spectrum - GC-MS (Non-derivatized) - 70eV, Positive | splash10-000f-9000000000-f5e8094c68372ab25a63 | 2017-09-01 | View Spectrum | | Predicted GC-MS | Predicted GC-MS Spectrum - GC-MS (2 TMS) - 70eV, Positive | splash10-00xr-9510000000-28b0e365a156d2091afd | 2017-10-06 | View Spectrum | | Predicted GC-MS | Predicted GC-MS Spectrum - GC-MS (Non-derivatized) - 70eV, Positive | Not Available | 2021-10-12 | View Spectrum | | LC-MS/MS | LC-MS/MS Spectrum - Quattro_QQQ 10V, Positive (Annotated) | splash10-00di-9000000000-cb3d53cc3c40c1cbbba7 | 2012-07-25 | View Spectrum | | LC-MS/MS | LC-MS/MS Spectrum - Quattro_QQQ 25V, Positive (Annotated) | splash10-0uk9-9000000000-53a009b344e3920ffca1 | 2012-07-25 | View Spectrum | | LC-MS/MS | LC-MS/MS Spectrum - Quattro_QQQ 40V, Positive (Annotated) | splash10-000i-9000000000-2bafb6c472ab1030cd0f | 2012-07-25 | View Spectrum | | LC-MS/MS | LC-MS/MS Spectrum - EI-B (Unknown) , Positive | splash10-0006-9000000000-8aef9a64d926571c2de0 | 2012-08-31 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 10V, Positive | splash10-0006-9000000000-d1ff7c94a720b1eecaf2 | 2015-04-24 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 20V, Positive | splash10-0006-9000000000-21d33d1d99d80526ee71 | 2015-04-24 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 40V, Positive | splash10-0006-9000000000-ac27102ff43446c313d3 | 2015-04-24 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 10V, Negative | splash10-000i-9000000000-fe58eaea122c39178fbe | 2015-04-25 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 20V, Negative | splash10-000i-9000000000-3850c6a7016e2874d55b | 2015-04-25 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 40V, Negative | splash10-000i-9000000000-32ac4118fe0eb9a5abb2 | 2015-04-25 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 10V, Negative | splash10-000i-9000000000-43de084d66dd1bebdeac | 2021-09-23 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 20V, Negative | splash10-000i-9000000000-159ed524013577f6f801 | 2021-09-23 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 40V, Negative | splash10-0006-9000000000-d948d5d95ae14e701f57 | 2021-09-23 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 10V, Positive | splash10-00di-9000000000-8e2d2f7a8acc88f00195 | 2021-09-25 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 20V, Positive | splash10-0006-9000000000-d7b47276d03e46ce72a2 | 2021-09-25 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 40V, Positive | splash10-0006-9000000000-a1e091bb1f5fa6e9cbc7 | 2021-09-25 | View Spectrum | | MS | Mass Spectrum (Electron Ionization) | splash10-0002-9000000000-538465f019815d5e1b4a | 2014-09-20 | View Spectrum | | 1D NMR | 13C NMR Spectrum (1D, 100 MHz, H2O, predicted) | Not Available | 2022-08-20 | View Spectrum | | 1D NMR | 13C NMR Spectrum (1D, 1000 MHz, H2O, predicted) | Not Available | 2022-08-20 | View Spectrum | | 1D NMR | 13C NMR Spectrum (1D, 200 MHz, H2O, predicted) | Not Available | 2022-08-20 | View Spectrum | | 1D NMR | 13C NMR Spectrum (1D, 300 MHz, H2O, predicted) | Not Available | 2022-08-20 | View Spectrum | | 1D NMR | 13C NMR Spectrum (1D, 400 MHz, H2O, predicted) | Not Available | 2022-08-20 | View Spectrum | | 1D NMR | 13C NMR Spectrum (1D, 500 MHz, H2O, predicted) | Not Available | 2022-08-20 | View Spectrum | | 1D NMR | 13C NMR Spectrum (1D, 600 MHz, H2O, predicted) | Not Available | 2022-08-20 | View Spectrum | | 1D NMR | 13C NMR Spectrum (1D, 700 MHz, H2O, predicted) | Not Available | 2022-08-20 | View Spectrum | | 1D NMR | 13C NMR Spectrum (1D, 800 MHz, H2O, predicted) | Not Available | 2022-08-20 | View Spectrum | | 1D NMR | 13C NMR Spectrum (1D, 900 MHz, H2O, predicted) | Not Available | 2022-08-20 | View Spectrum |
|
|---|
| Toxicity Profile |
|---|
| Route of Exposure | Not Available |
|---|
| Mechanism of Toxicity | The affinity of divalent metal ions is sometimes reflected in their tendency to form insoluble precipitates. Thus in the body, oxalic acid also combines with metals ions such as Ca2+, Fe2+, and Mg2+ to deposit crystals of the corresponding oxalates, which irritate the gut and kidneys. (2) Therefore the toxicity of oxalic acid is due to kidney failure caused by precipitation of solid calcium oxalate, the main component of kidney stones. Oxalic acid can also cause joint pain due to the formation of similar precipitates in the joints. Ingestion of ethylene glycol results in oxalic acid as a metabolite that can also cause acute kidney failure. |
|---|
| Metabolism | Oxalic acid is not metabolized but excreted in the urine. |
|---|
| Toxicity Values | Not Available |
|---|
| Lethal Dose | Oral LDLo (lowest published lethal dose) of 600 mg/kg. It has been reported that the lethal oral dose is 15 to 30 grams. |
|---|
| Carcinogenicity (IARC Classification) | No indication of carcinogenicity (not listed by IARC). (23) |
|---|
| Uses/Sources | Oxalic acid and oxalates are abundantly present in many plants, most notably fat hen (lamb's quarters), sorrel, and Oxalis species. The root and/or leaves of rhubarb and buckwheat are listed being high in oxalic acid.[8] Other edible plants that contain significant concentrations of oxalic acid include—in decreasing order—star fruit (carambola), black pepper, parsley, poppy seed, amaranth, spinach, chard, beets, cocoa, chocolate, most nuts, most berries, and beans. (22) |
|---|
| Minimum Risk Level | Not Available |
|---|
| Health Effects | Because it binds vital nutrients such as calcium, long-term consumption of foods high in oxalic acid can be problematic. Healthy individuals can safely consume such foods in moderation, but those with kidney disorders, gout, rheumatoid arthritis, or certain forms of chronic vulvar pain (vulvodynia) are typically advised to avoid foods high in oxalic acid or oxalates. The calcium oxalate precipitate (better known as kidney stones) obstruct the kidney tubules. Conversely, calcium supplements taken along with foods high in oxalic acid can cause calcium oxalate to precipitate out in the gut and drastically reduce the levels of oxalate absorbed by the body (by 97% in some cases.)
Chronically high levels of oxalic acid are associated with at least 2 inborn errors of metabolism including: Type I primary hyperoxaluria and Primary hyperoxaluria. Oxalate stones in primary hyperoxaluria tend to be severe, resulting in relatively early kidney damage (before age 20), which impairs the excretion of oxalate leading to a further acceleration in accumulation of oxalate in the body. After the development of renal failure patients may develop oxalate deposits in the bones, joints and bone marrow. Severe cases may develop haematological problems such as anaemia and thrombocytopaenia. The deposition of oxalate in the body is sometimes called "oxalosis" to be distinguished from "oxaluria" which refers to oxalate in the urine. |
|---|
| Symptoms | Oxalic acid poisoning symptoms include weakness, burning in the mouth, death from cardiovascular collapse, on the respiratory system, throat – burning in the throat, abdominal pain, nausea, vomiting, diarrhea, convulsions, and coma. |
|---|
| Treatment | Acute Exposure: If oxalic acid is swallowed, immediately give the person water or milk, unless instructed otherwise by a health care provider. DO NOT give water or milk if the person is having symptoms (such as vomiting, convulsions, or a decreased level of alertness) that make it hard to swallow. If acute exposure occurs to the eyes, irrigate opened eyes for several minutes under running water.
Chronic exposure: in some patients with primary hyperoxaluria type 1, pyridoxine treatment (vitamin B6) may decrease oxalate excretion and prevent kidney stone formation. |
|---|
| Normal Concentrations |
|---|
| Not Available |
|---|
| Abnormal Concentrations |
|---|
| Not Available |
|---|
| External Links |
|---|
| DrugBank ID | DB03902 |
|---|
| HMDB ID | HMDB02329 |
|---|
| PubChem Compound ID | 971 |
|---|
| ChEMBL ID | CHEMBL146755 |
|---|
| ChemSpider ID | 946 |
|---|
| KEGG ID | C00209 |
|---|
| UniProt ID | Not Available |
|---|
| OMIM ID | 109600 , 138500 , 167030 , 240400 , 259900 , 260000 , 260005 |
|---|
| ChEBI ID | 16995 |
|---|
| BioCyc ID | CUPRIZONE |
|---|
| CTD ID | D019815 |
|---|
| Stitch ID | Oxalic Acid |
|---|
| PDB ID | OXD |
|---|
| ACToR ID | 3709 |
|---|
| Wikipedia Link | Oxalic acid |
|---|
| References |
|---|
| Synthesis Reference | Giuseppe Messina, Giovanni M. Sechi, Loreno Lorenzoni, Giovanni Chessa, “Method of preparation of oxalic acid esters and amides.” U.S. Patent US4981963, issued July, 1971. |
|---|
| MSDS | Link |
|---|
| General References | - de O G Mendonca C, Martini LA, Baxmann AC, Nishiura JL, Cuppari L, Sigulem DM, Heilberg IP: Effects of an oxalate load on urinary oxalate excretion in calcium stone formers. J Ren Nutr. 2003 Jan;13(1):39-46. [12563622 ]
- Singh S, Tai C, Ganz G, Yeung CK, Magil A, Rosenberg F, Applegarth D, Levin A: Steroid-responsive pleuropericarditis and livedo reticularis in an unusual case of adult-onset primary hyperoxaluria. Am J Kidney Dis. 1999 Apr;33(4):e5. [10196036 ]
- Astarcioglu I, Karademir S, Gulay H, Bora S, Astarcioglu H, Kavukcu S, Turkmen M, Soylu A: Primary hyperoxaluria: simultaneous combined liver and kidney transplantation from a living related donor. Liver Transpl. 2003 Apr;9(4):433-6. [12682898 ]
- Selvam R, Kalaiselvi P: A novel basic protein from human kidney which inhibits calcium oxalate crystal growth. BJU Int. 2000 Jul;86(1):7-13. [10886075 ]
- Kwak C, Jeong BC, Kim HK, Kim EC, Chox MS, Kim HH: Molecular epidemiology of fecal Oxalobacter formigenes in healthy adults living in Seoul, Korea. J Endourol. 2003 May;17(4):239-43. [12816588 ]
- Vicanova J, Boelsma E, Mommaas AM, Kempenaar JA, Forslind B, Pallon J, Egelrud T, Koerten HK, Ponec M: Normalization of epidermal calcium distribution profile in reconstructed human epidermis is related to improvement of terminal differentiation and stratum corneum barrier formation. J Invest Dermatol. 1998 Jul;111(1):97-106. [9665394 ]
- Mydlik M, Derzsiova K, Pribylincova V, Reznicek J: [Urinary oxalic acid excretion in chronic kidney failure and after kidney transplantation]. Vnitr Lek. 1996 Dec;42(12):813-7. [9072879 ]
- Mizusawa Y, Parnham AP, Falk MC, Burke JR, Nicol D, Yamanaka J, Lynch SV, Strong RW: Potential for bilateral nephrectomy to reduce oxalate release after combined liver and kidney transplantation for primary hyperoxaluria type 1. Clin Transplant. 1997 Oct;11(5 Pt 1):361-5. [9361924 ]
- Pecorella I, McCartney AC, Lucas S, Michaels L, Ciardi A, Di Tondo U, Garner A: Histological study of oxalosis in the eye and adnexa of AIDS patients. Histopathology. 1995 Nov;27(5):431-8. [8575733 ]
- Huang MY, Chaturvedi LS, Koul S, Koul HK: Oxalate stimulates IL-6 production in HK-2 cells, a line of human renal proximal tubular epithelial cells. Kidney Int. 2005 Aug;68(2):497-503. [16014026 ]
- Shapiro R, Weismann I, Mandel H, Eisenstein B, Ben-Ari Z, Bar-Nathan N, Zehavi I, Dinari G, Mor E: Primary hyperoxaluria type 1: improved outcome with timely liver transplantation: a single-center report of 36 children. Transplantation. 2001 Aug 15;72(3):428-32. [11502971 ]
- Motoyoshil Y, Hattori M, Chikamoto H, Nakakura H, Furue T, Miyakawa S, Kohno M, Ito K, Kai K, Nakajima I, Fuchinoue S, Teraoka S, Akiba T, Kitayama H, Wada N, Ogawa Y: [Sequential combined liver-kidney transplantation for a one-year-old boy with infantile primary hyperoxaluria type 1]. Nihon Jinzo Gakkai Shi. 2006;48(1):22-8. [16480063 ]
- de Water R, Noordermeer C, van der Kwast TH, Nizze H, Boeve ER, Kok DJ, Schroder FH: Calcium oxalate nephrolithiasis: effect of renal crystal deposition on the cellular composition of the renal interstitium. Am J Kidney Dis. 1999 Apr;33(4):761-71. [10196021 ]
- van Woerden CS, Groothof JW, Wanders RJ, Waterham HR, Wijburg FR: [From gene to disease; primary hyperoxaluria type I caused by mutations in the AGXT gene]. Ned Tijdschr Geneeskd. 2006 Jul 29;150(30):1669-72. [16922352 ]
- Pirulli D, Marangella M, Amoroso A: Primary hyperoxaluria: genotype-phenotype correlation. J Nephrol. 2003 Mar-Apr;16(2):297-309. [12768081 ]
- Amoroso A, Pirulli D, Florian F, Puzzer D, Boniotto M, Crovella S, Zezlina S, Spano A, Mazzola G, Savoldi S, Ferrettini C, Berutti S, Petrarulo M, Marangella M: AGXT gene mutations and their influence on clinical heterogeneity of type 1 primary hyperoxaluria. J Am Soc Nephrol. 2001 Oct;12(10):2072-9. [11562405 ]
- Robertson WG: Renal stones in the tropics. Semin Nephrol. 2003 Jan;23(1):77-87. [12563603 ]
- Nakagawa Y, Abram V, Parks JH, Lau HS, Kawooya JK, Coe FL: Urine glycoprotein crystal growth inhibitors. Evidence for a molecular abnormality in calcium oxalate nephrolithiasis. J Clin Invest. 1985 Oct;76(4):1455-62. [4056037 ]
- Massey LK, Palmer RG, Horner HT: Oxalate content of soybean seeds (Glycine max: Leguminosae), soyfoods, and other edible legumes. J Agric Food Chem. 2001 Sep;49(9):4262-6. [11559120 ]
- Petrarulo M, Vitale C, Facchini P, Marangella M: Biochemical approach to diagnosis and differentiation of primary hyperoxalurias: an update. J Nephrol. 1998 Mar-Apr;11 Suppl 1:23-8. [9604805 ]
- New Zealand Food Safety Authority (2009). Natural Toxins In Food. [Link]
- Wikipedia. Oxalic Acid. Last Updated 20 April 2009. [Link]
- International Agency for Research on Cancer (2014). IARC Monographs on the Evaluation of Carcinogenic Risks to Humans. [Link]
|
|---|
| Gene Regulation |
|---|
| Up-Regulated Genes | | Gene | Gene Symbol | Gene ID | Interaction | Chromosome | Details |
|---|
|
|---|
| Down-Regulated Genes | Not Available |
|---|