| Record Information |
|---|
| Version | 2.0 |
|---|
| Creation Date | 2009-07-21 20:28:09 UTC |
|---|
| Update Date | 2014-12-24 20:25:54 UTC |
|---|
| Accession Number | T3D2955 |
|---|
| Identification |
|---|
| Common Name | Levobupivacaine |
|---|
| Class | Small Molecule |
|---|
| Description | Levobupivacaine is an amino-amide local anaesthetic drug belonging to the family of n-alkylsubstituted pipecoloxylidide. It is the S-enantiomer of bupivacaine. Levobupivacaine hydrochloride is commonly marketed by AstraZeneca under the trade name Chirocaine. Compared to bupivacaine, levobupivacaine is associated with less vasodilation and has a longer duration of action. It is approximately 13 per cent less potent (by molarity) than racemic bupivacaine.Levobupivacaine is indicated for local anaesthesia including infiltration, nerve block, ophthalmic, epidural and intrathecal anaesthesia in adults; and infiltration analgesia in children. Adverse drug reactions (ADRs) are rare when it is administered correctly. Most ADRs relate to administration technique (resulting in systemic exposure) or pharmacological effects of anesthesia, however allergic reactions can rarely occur. [Wikipedia] |
|---|
| Compound Type | - Amide
- Amine
- Anesthetic
- Anesthetic, Local
- Drug
- Metabolite
- Organic Compound
- Synthetic Compound
|
|---|
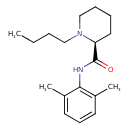
| Chemical Structure | |
|---|
| Synonyms | | Synonym | | (-)-Bupivacaine | | (S)-1-Butyl-2',6'-pipecoloxylidide | | (S)-Bupivacaine | | Chirocaine | | L-(-)-1-Butyl-2',6'-pipecoloxylidide | | L-(-)-Bupivacaine | | Levobupivacaine hydrochloride |
|
|---|
| Chemical Formula | C18H28N2O |
|---|
| Average Molecular Mass | 288.428 g/mol |
|---|
| Monoisotopic Mass | 288.220 g/mol |
|---|
| CAS Registry Number | 27262-47-1 |
|---|
| IUPAC Name | (2S)-1-butyl-N-(2,6-dimethylphenyl)piperidine-2-carboxamide |
|---|
| Traditional Name | (-)-bupivacaine |
|---|
| SMILES | [H][C@]1(CCCCN1CCCC)C(O)=NC1=C(C)C=CC=C1C |
|---|
| InChI Identifier | InChI=1S/C18H28N2O/c1-4-5-12-20-13-7-6-11-16(20)18(21)19-17-14(2)9-8-10-15(17)3/h8-10,16H,4-7,11-13H2,1-3H3,(H,19,21)/t16-/m0/s1 |
|---|
| InChI Key | InChIKey=LEBVLXFERQHONN-INIZCTEOSA-N |
|---|
| Chemical Taxonomy |
|---|
| Description | belongs to the class of organic compounds known as piperidinecarboxamides. Piperidinecarboxamides are compounds containing a piperidine ring substituted with a carboxamide functional group. |
|---|
| Kingdom | Organic compounds |
|---|
| Super Class | Organoheterocyclic compounds |
|---|
| Class | Piperidines |
|---|
| Sub Class | Piperidinecarboxylic acids and derivatives |
|---|
| Direct Parent | Piperidinecarboxamides |
|---|
| Alternative Parents | |
|---|
| Substituents | - 2-piperidinecarboxamide
- Piperidinecarboxamide
- M-xylene
- Xylene
- Monocyclic benzene moiety
- Benzenoid
- Tertiary aliphatic amine
- Tertiary amine
- Carboximidic acid
- Carboximidic acid derivative
- Azacycle
- Organic 1,3-dipolar compound
- Propargyl-type 1,3-dipolar organic compound
- Amine
- Hydrocarbon derivative
- Organooxygen compound
- Organonitrogen compound
- Organopnictogen compound
- Organic oxygen compound
- Organic nitrogen compound
- Aromatic heteromonocyclic compound
|
|---|
| Molecular Framework | Aromatic heteromonocyclic compounds |
|---|
| External Descriptors | - 1-butyl-N-(2,6-dimethylphenyl)piperidine-2-carboxamide (CHEBI:6149 )
|
|---|
| Biological Properties |
|---|
| Status | Detected and Not Quantified |
|---|
| Origin | Exogenous |
|---|
| Cellular Locations | |
|---|
| Biofluid Locations | Not Available |
|---|
| Tissue Locations | Not Available |
|---|
| Pathways | | Name | SMPDB Link | KEGG Link |
|---|
| Levobupivacaine Pathway | Not Available | Not Available |
|
|---|
| Applications | |
|---|
| Biological Roles | |
|---|
| Chemical Roles | |
|---|
| Physical Properties |
|---|
| State | Solid |
|---|
| Appearance | White powder. |
|---|
| Experimental Properties | | Property | Value |
|---|
| Melting Point | Not Available | | Boiling Point | Not Available | | Solubility | 9.77e-02 g/L | | LogP | 3.6 |
|
|---|
| Predicted Properties | |
|---|
| Spectra |
|---|
| Spectra | | Spectrum Type | Description | Splash Key | Deposition Date | View |
|---|
| Predicted GC-MS | Predicted GC-MS Spectrum - GC-MS (Non-derivatized) - 70eV, Positive | splash10-006t-6920000000-20e4e8d5c09a52a31c75 | 2017-09-01 | View Spectrum | | Predicted GC-MS | Predicted GC-MS Spectrum - GC-MS (Non-derivatized) - 70eV, Positive | Not Available | 2021-10-12 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 10V, Positive | splash10-0079-0970000000-e665f05dc8da9fafd8f0 | 2016-08-03 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 20V, Positive | splash10-00dl-2900000000-6396ddc6fc9d5e9b6c64 | 2016-08-03 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 40V, Positive | splash10-0ac0-9200000000-befeaee90e72918d68b3 | 2016-08-03 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 10V, Negative | splash10-000i-0290000000-e01610a30f93d9c5ec2a | 2016-08-03 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 20V, Negative | splash10-00ri-0970000000-e26949f880557c6da815 | 2016-08-03 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 40V, Negative | splash10-00xr-3900000000-56dfe5d9cd7f629f17e3 | 2016-08-03 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 10V, Negative | splash10-000i-0090000000-e83ab5b70775090159b7 | 2021-10-11 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 20V, Negative | splash10-000i-0690000000-6ff0193988455d286726 | 2021-10-11 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 40V, Negative | splash10-00xr-1920000000-87f1897c4a60793791d5 | 2021-10-11 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 10V, Positive | splash10-000i-0190000000-23ffc562239624515183 | 2021-10-11 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 20V, Positive | splash10-000g-3920000000-6aaf7d8f5f0149cec33e | 2021-10-11 | View Spectrum | | Predicted LC-MS/MS | Predicted LC-MS/MS Spectrum - 40V, Positive | splash10-0007-8900000000-e62af4b8065c6c1caf01 | 2021-10-11 | View Spectrum |
|
|---|
| Toxicity Profile |
|---|
| Route of Exposure | The plasma concentration of levobupivacaine following therapeutic administration depends on dose and also on route of administration, because absorption from the site of administration is affected by the vascularity of the tissue. Peak levels in blood were reached approximately 30 minutes after epidural administration, and doses up to 150 mg resulted in mean Cmax levels of up to 1.2 ug/mL. |
|---|
| Mechanism of Toxicity | Levobupivacaine is a cholinesterase or acetylcholinesterase (AChE) inhibitor. A cholinesterase inhibitor (or 'anticholinesterase') suppresses the action of acetylcholinesterase. Because of its essential function, chemicals that interfere with the action of acetylcholinesterase are potent neurotoxins, causing excessive salivation and eye-watering in low doses, followed by muscle spasms and ultimately death. Nerve gases and many substances used in insecticides have been shown to act by binding a serine in the active site of acetylcholine esterase, inhibiting the enzyme completely. Acetylcholine esterase breaks down the neurotransmitter acetylcholine, which is released at nerve and muscle junctions, in order to allow the muscle or organ to relax. The result of acetylcholine esterase inhibition is that acetylcholine builds up and continues to act so that any nerve impulses are continually transmitted and muscle contractions do not stop. Among the most common acetylcholinesterase inhibitors are phosphorus-based compounds, which are designed to bind to the active site of the enzyme. The structural requirements are a phosphorus atom bearing two lipophilic groups, a leaving group (such as a halide or thiocyanate), and a terminal oxygen. |
|---|
| Metabolism | Levobupivacaine is extensively metabolized with no unchanged levobupivacaine detected in urine or feces. In vitro studies using [14 C] levobupivacaine showed that CYP3A4 isoform and CYP1A2 isoform mediate the metabolism of levobupivacaine to desbutyl levobupivacaine and 3-hydroxy levobupivacaine, respectively. In vivo, the 3-hydroxy levobupivacaine appears to undergo further transformation to glucuronide and sulfate conjugates. Metabolic inversion of levobupivacaine to R(+)-bupivacaine was not evident both in vitro and in vivo.
Route of Elimination: Following intravenous administration, recovery of the radiolabelled dose of levobupivacaine was essentially quantitative with a mean total of about 95% being recovered in urine and feces in 48 hours. Of this 95%, about 71% was in urine while 24% was in feces.
Half Life: 3.3 hours |
|---|
| Toxicity Values | LD50: 5.1mg/kg in rabbit, intravenous; 18mg/kg in rabbit, oral; 207mg/kg in rabbit, parenteral; 63mg/kg in rat, subcutaneous. |
|---|
| Lethal Dose | Not Available |
|---|
| Carcinogenicity (IARC Classification) | No indication of carcinogenicity to humans (not listed by IARC). |
|---|
| Uses/Sources | For the production of local or regional anesthesia for surgery and obstetrics, and for post-operative pain management |
|---|
| Minimum Risk Level | Not Available |
|---|
| Health Effects | Acute exposure to cholinesterase inhibitors can cause a cholinergic crisis characterized by severe nausea/vomiting, salivation, sweating, bradycardia, hypotension, collapse, and convulsions. Increasing muscle weakness is a possibility and may result in death if respiratory muscles are involved. Accumulation of ACh at motor nerves causes overstimulation of nicotinic expression at the neuromuscular junction. When this occurs symptoms such as muscle weakness, fatigue, muscle cramps, fasciculation, and paralysis can be seen. When there is an accumulation of ACh at autonomic ganglia this causes overstimulation of nicotinic expression in the sympathetic system. Symptoms associated with this are hypertension, and hypoglycemia. Overstimulation of nicotinic acetylcholine receptors in the central nervous system, due to accumulation of ACh, results in anxiety, headache, convulsions, ataxia, depression of respiration and circulation, tremor, general weakness, and potentially coma. When there is expression of muscarinic overstimulation due to excess acetylcholine at muscarinic acetylcholine receptors symptoms of visual disturbances, tightness in chest, wheezing due to bronchoconstriction, increased bronchial secretions, increased salivation, lacrimation, sweating, peristalsis, and urination can occur. Certain reproductive effects in fertility, growth, and development for males and females have been linked specifically to organophosphate pesticide exposure. Most of the research on reproductive effects has been conducted on farmers working with pesticides and insecticdes in rural areas. In females menstrual cycle disturbances, longer pregnancies, spontaneous abortions, stillbirths, and some developmental effects in offspring have been linked to organophosphate pesticide exposure. Prenatal exposure has been linked to impaired fetal growth and development. Neurotoxic effects have also been linked to poisoning with OP pesticides causing four neurotoxic effects in humans: cholinergic syndrome, intermediate syndrome, organophosphate-induced delayed polyneuropathy (OPIDP), and chronic organophosphate-induced neuropsychiatric disorder (COPIND). These syndromes result after acute and chronic exposure to OP pesticides. |
|---|
| Symptoms | nervousness, tingling around the mouth, tinnitus, tremor, dizziness, blurred vision, seizures, depression (drowsiness, loss of consciousness, respiratory depression and apnea). [Wikipedia] |
|---|
| Treatment | If the compound has been ingested, rapid gastric lavage should be performed using 5% sodium bicarbonate. For skin contact, the skin should be washed with soap and water. If the compound has entered the eyes, they should be washed with large quantities of isotonic saline or water. In serious cases, atropine and/or pralidoxime should be administered. Anti-cholinergic drugs work to counteract the effects of excess acetylcholine and reactivate AChE. Atropine can be used as an antidote in conjunction with pralidoxime or other pyridinium oximes (such as trimedoxime or obidoxime), though the use of '-oximes' has been found to be of no benefit, or possibly harmful, in at least two meta-analyses. Atropine is a muscarinic antagonist, and thus blocks the action of acetylcholine peripherally. |
|---|
| Normal Concentrations |
|---|
| Not Available |
|---|
| Abnormal Concentrations |
|---|
| Not Available |
|---|
| External Links |
|---|
| DrugBank ID | DB01002 |
|---|
| HMDB ID | HMDB15137 |
|---|
| PubChem Compound ID | 92253 |
|---|
| ChEMBL ID | CHEMBL1201193 |
|---|
| ChemSpider ID | 83289 |
|---|
| KEGG ID | C07887 |
|---|
| UniProt ID | Not Available |
|---|
| OMIM ID | |
|---|
| ChEBI ID | 6149 |
|---|
| BioCyc ID | Not Available |
|---|
| CTD ID | Not Available |
|---|
| Stitch ID | Levobupivacaine |
|---|
| PDB ID | Not Available |
|---|
| ACToR ID | Not Available |
|---|
| Wikipedia Link | Levobupivacaine |
|---|
| References |
|---|
| Synthesis Reference | Hooshang Shahriari Zavareh, Graham Anthony Charles Frampton, “Process for preparing levobupivacaine and analogues thereof.” U.S. Patent US5777124, issued February, 1985. |
|---|
| MSDS | Not Available |
|---|
| General References | - Burlacu CL, Buggy DJ: Update on local anesthetics: focus on levobupivacaine. Ther Clin Risk Manag. 2008 Apr;4(2):381-92. [18728849 ]
- Leone S, Di Cianni S, Casati A, Fanelli G: Pharmacology, toxicology, and clinical use of new long acting local anesthetics, ropivacaine and levobupivacaine. Acta Biomed. 2008 Aug;79(2):92-105. [18788503 ]
- Drugs.com [Link]
- Gaval-Cruz M, Weinshenker D: mechanisms of disulfiram-induced cocaine abstinence: antabuse and cocaine relapse. Mol Interv. 2009 Aug;9(4):175-87. [Link]
- http://www.orgyn.com/resources/genrx/D003445.asp [Link]
|
|---|
| Gene Regulation |
|---|
| Up-Regulated Genes | Not Available |
|---|
| Down-Regulated Genes | Not Available |
|---|